DexCom: Innovative Diabetes Management

This article was written on July 8, 2020.
DexCom is a leading medical device company primarily focused on the design, development, and commercialization of continuous glucose monitoring (CGM) systems for individuals with diabetes.
Diabetes is one of the most disruptive markets in medical technology driven by the rapid pace of product innovation that is transforming the diabetes device and technology market. Fueling this growth is the substantial increase of diabetes globally and faster FDA approvals as regulators and payers are realizing the risks and costs of under-management of this disease.
We believe the market is under-estimating the potential acceleration in CGM adoption as the standard of care for blood sugar (glucose) monitoring compared to the traditional method of fingersticks. Clinical research shows that CGM technology contributes to better glycemic outcomes and improved diabetes treatment decisions by delivering patients blood glucose readings in real-time.
We believe DexCom will be a prime beneficiary of the increasing awareness of improved diabetes management technology and the rapid shift to telehealth and remote monitoring as leading factors driving CGM adoption.
What is Diabetes?
Diabetes is a chronic life threatening disease where your body is unable to produce sufficient insulin or fails to properly use the insulin it produces. Insulin is a hormone created by the pancreas that regulates the body’s blood sugar levels.
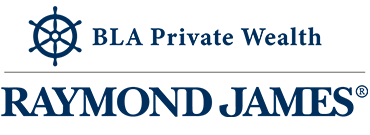
The International Diabetes Foundation (IDF) estimates that in 2019, 463 million adults (aged 20 to 79) around the world had diabetes, including 31 million in the U.S. By 2045, the number of people with diabetes is expected to increase to 700 million [1].
Source: DexCom April 2020 presentation
Diabetes is classified into two groups: type 1 diabetes and type 2 diabetes.
- Type 1 diabetes is an autoimmune disease characterized by an absence of insulin. This type of diabetes occurs when the immune system attacks and destroys the cells in the pancreas that produce insulin. People with type 1 diabetes must rely on regular insulin injections or infusions via syringe or insulin pump to regulate blood sugar levels.
- Type 2 diabetes is a metabolic disease characterized by insulin resistance and relative insulin deficiency. In this case, the pancreas may still produce insulin, but the body’s cells start to resist the normal effects of insulin. As the body becomes more insulin resistant, the pancreas is forced to produce more and more insulin until the cells in the pancreas cannot keep up. Eventually the cells stop responding to insulin.
The inability to make or use insulin prevents the body from controlling blood glucose and leads to consistently high or low blood sugar levels.
The increase in blood sugar levels above the normal range is called hyperglycemia. Hyperglycemia can result in long-term complications such as heart disease, kidney failure, and blindness. When blood sugar levels are high, people with diabetes often inject or pump insulin into their body to decrease blood sugar levels. The decrease in blood sugar levels below the normal range is called hypoglycemia. Hypoglycemia can result in complications such as loss of consciousness and seizures.
Many factors can affect your blood sugar levels including the carbohydrate and fat content of meals, exercise, stress, and the change of insulin in your body. It can be difficult to maintain blood sugar levels within a normal range. As a result, many people with diabetes experience frequent and unpredictable fluctuations between hyperglycemic and hypoglycemic states during the same day.
Fingerstick Glucose Monitoring
An important component of effective diabetes management is frequent monitoring of blood sugar levels. The American Diabetes Association recommends people with type 1 diabetes to measure their blood sugar levels at least three or more times daily.
Fingerstick testing is the most common for blood sugar monitoring and treating insulin dependent diabetes. This procedure involves manually pricking one’s finger with a small needle or lancet to obtain a small quantity of blood for testing. The pin-prick of blood is added to a test strip and inserted into a glucose meter to measure the individual’s blood sugar value.
However, there are a number of limitations and inconveniences to fingersticks. Blood glucose meters will only display a reading from a fingerstick at a single point in time. Patients are left with no understanding of their daily blood sugar trends which can fluctuate significantly between insulin doses and meals. There are no alarms or alerts to signal when blood sugar levels are too high or too low.
Moreover, the pain and discomfort of finger-pricking three or more times a day can disrupt one’s daily activities.
Continuous Glucose Monitoring
Continuous glucose monitoring (CGM) is a new technology to measure blood sugar levels multiple times throughout the day and night. CGM uses a patch device that is often placed on the abdomen or back of the arm to measure blood sugar at regular intervals and convert the data into actionable information for the patient. A slim sensor sits just under the skin and sends blood sugar levels wirelessly to a mobile device for real-time monitoring. Over the years, there has been an increase in uptake of CGMs among people with type 1 and type 2 diabetes as the devices have become smaller, user-friendly, and more accurate.
DexCom CGM devices such as the G6 measures blood sugar levels every five minutes. This gives patient’s access to valuable real-time glucose trends that they can then share with their doctor to receive medical advice and diagnosis. The device features alerts and alarms to notify users when blood sugar levels are too high or too low even when the patient is asleep.
Clinical studies show that patients spend less time in hyperglycemia and hypoglycemia when they use a DexCom CGM system compared to patients relying solely on single-point fingerstick measurements.
“In 2016, the first randomized, controlled study focusing solely on the benefit of continuous glucose monitoring for diabetes patients using multiple daily injections insulin therapy showed DexCom CGM system users on multiple daily injections of insulin therapy achieved a one percent average A1c reduction after 24 weeks of regular use, compared to their baseline. Study participants also increased time spent in their target A1c range and spent less time in hypoglycemia and hyperglycemia when they used a DexCom CGM system compared to those who used only a standard blood glucose meter to monitor their glucose.” – DexCom 2019 Annual Report
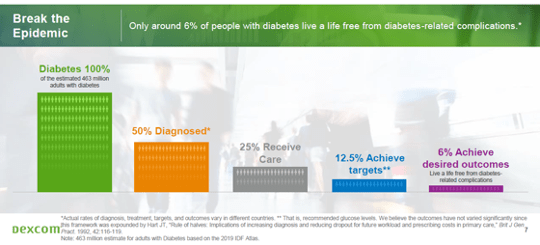
All in all, CGM improves glycemic outcomes and lowers the risk of long-term health complications associated with diabetes. The chart below shows the potential runway for CGM penetration to replace fingersticks for measuring blood glucose (BG) among people with intensively managed type 1 and type 2 diabetes in the U.S. [2].
DexCom’s Large Market Opportunity
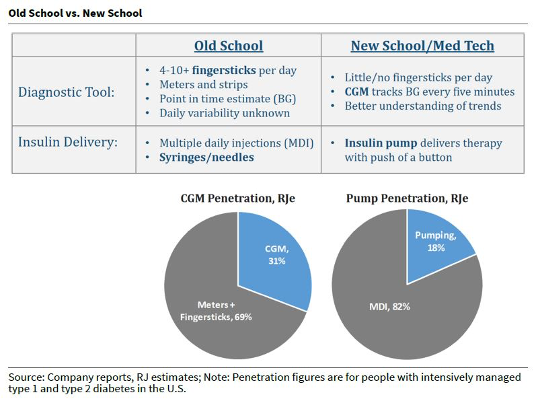
DexCom’s primary market consists of ~3.2 million insulin intensive patients in the U.S. These are patients with type 1 and type 2 diabetes on insulin pumps or multiple daily insulin injections. DexCom estimates CGM penetration has increased into the 35% to 40% range among type 1s and 15% among type 2s due to the growth of wearable and mobile technology, as well as gradual improvements in insurance coverage [3]. As CGM becomes a standard of care option, DexCom believes that 80% market penetration is possible for CGM devices in the U.S.
The core intensive diabetes market is an important revenue opportunity for the next few years, but the future and much larger opportunity lies in the non-insulin intensive diabetes market. CGM devices are expected to expand into larger under-penetrated populations in the U.S., including the gestational diabetes market (~4 million patients), the non-intensive type 2 diabetes market (~27 million patients), and the pre-diabetes markets (~84 million patients at risk of developing type 2 diabetes) [4].
Lastly, CGM technology can be expanded into the hospital setting as a disease management tool for in-hospital patients experiencing all types and levels of dysglycemia (abnormal blood sugar activity) due to diabetes and other health conditions. DexCom sizes the U.S. hospital end market at ~14 million patients. If the patient experiences hyperglycemia or hypoglycemia while in the hospital (both of which are preventable), there is a higher rate of readmission within 30 days of discharge. This represents a high cost burden for insurers and the health care system.
“Approximately 30% of all health care expenditures incurred by people with diabetes come from higher rates of hospital admission and longer average lengths of stay per admission, constituting the single largest contributor to the medical cost of diabetes. Of the $486 billion in national expenditures for hospital inpatient care in 2017, approximately $123 billion is incurred by people who have diabetes, of which $70 billion is directly attributed to their diabetes.” – DexCom 2019 Annual Report
According to the American Diabetes Association, one in every four health care dollars was spent on treating people with diabetes in 2017. We believe DexCom has a solid CGM system that can improve the management of diabetes and lower the costs incurred by insurers and the health care system. Our discussion and the table below highlight the U.S. patient opportunity, but the international patient opportunity is much larger, and provides DexCom a long growth runway for several years.
Final remarks
In fiscal 2019, DexCom reported its first full year of profitability on revenue growth of 43%, which consisted of U.S. revenue growth of 42% and international revenue growth of 48%. New patients are the primary driver behind the growth. DexCom ended the year approaching ~650,000 net active patients globally [5]. DexCom is uniquely positioned to benefit from the rising adoption of continuous glucose monitoring (CGM) to manage type 1 diabetes and insulin-requiring type 2 diabetes. Non-intensive individuals with diabetes such as non-intensive type 2 diabetes and pre-diabetes are coming into focus and should provide strong growth for DexCom over the long term.
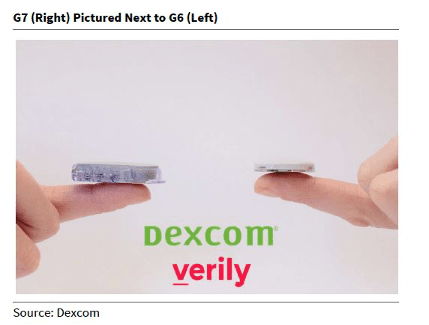
An important growth driver will be the commercial launch of DexCom’s next gen G7 CGM platform in 2021 (see image below). The G7 is much thinner, less expensive, and fully disposable, thus making it more suitable for hospital inventory and more affordable for people in the broader non-intensive diabetes and pre-diabetes markets. In the U.S., DexCom is making inroads into the pharmacy channel, which the company expects will enable easier, quicker, and affordable access for CGMs, both for people with type 1 and type 2 diabetes on insulin, as well as the non-intensive diabetes markets. Overall, the broader acceptance of CGM and the sizable global market should provide a strong growth runway for DexCom in front of the G7 launch.
We have an optimistic outlook on the diabetes market. We view it as one of the top themes in medical technology as new insulin pump and CGM technology replaces old syringe and fingerstick testing.
Sources
- DexCom 2019 Annual Report.
- Raymond James. Diabetes Deep-Dive, the Continued Evolution (and Acceptance) of New Diabetes Tech. February 5, 2020.
- April 2020 presentation.
- Investor Day 2018 presentation.
- DexCom (DXCM) Q4 2019 Earnings Call Transcript. [LINK]
Information in this article is from sources believed to be reliable; however, we cannot represent that it is accurate or complete. It is provided as a general source of information and should not be considered personal investment advice or solicitation to buy or sell securities. The views are those of the author, Christopher De Sousa, and not necessarily those of Raymond James Ltd. Investors considering any investment should consult with their Investment Advisor to ensure that it is suitable for the investor’s circumstances and risk tolerance before making any investment decision. Raymond James Ltd. is a Member Canadian Investor Protection Fund.